Signed in as:
filler@godaddy.com
Signed in as:
filler@godaddy.com
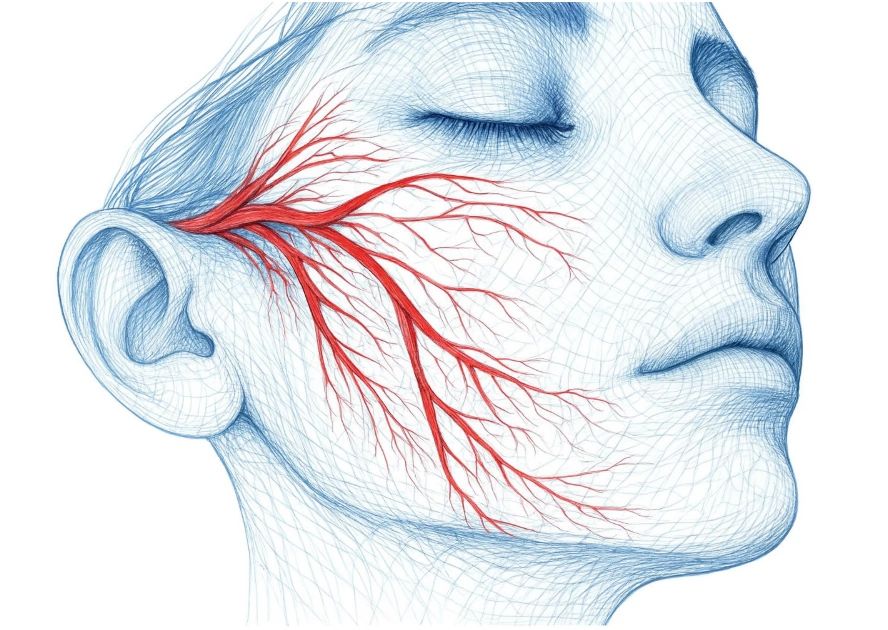
Vasodilation means your blood vessels widen, allowing more blood to flow to the skin. This helps deliver more oxygen and nutrients to skin cells, which can support collagen production and keep your skin healthy. While vasodilation does not create collagen, it creates the ideal environment to repair and renew itself.
Wong, Q.Y.A., Chew, F.T. Defining skin aging and its risk factors: a systematic review and meta-analysis. Sci Rep 11, 22075 (2021). https://doi.org/10.1038/s41598-021-01573-z
Ganceviciene R, Liakou AI, Theodoridis A, Makrantonaki E, Zouboulis CC. Skin anti-aging strategies. Dermatoendocrinol. 2012 Jul 1;4(3):308-19. doi: 10.4161/derm.22804. PMID: 23467476; PMCID: PMC3583892.
1. Basic Clinical Observation
2. Contributing Factors
3. Commonly Referenced Tools
4. Clinical & Preventive Considerations
1. Basic Clinical Observation
2. Contributing Factors
3. Commonly Referenced Assessment Tools
4. Clinical & Preventive Considerations
1. Basic Clinical Observation
Visual Inspection:Enlarged pores appear as small openings on the skin surface, most
noticeable on the nose, cheeks, and forehead.
Characteristics:
2. Contributing Factors
3. Commonly Referenced Tools
4. Clinical & Preventive Considerations
Prevention (general measures):
Management (commonly referenced in dermatology):
Supportive care: Thermal-based devices (e.g., VASO Mask) may be incorporated as adjunctive
care to support circulation and overall skin condition.
1. Basic Clinical Observation
Visual Inspection:Assess the distribution, intensity, and pattern of dyspigmentation (e.g.,
freckles, melasma, sunspots, age spots).
Classification (commonly referenced in dermatology):
Pattern & Localization:
2. Factors Contributing to Dyspigmentation
3. Professional Assessment Tools
4. Clinical Recommendations
Prevention (widely recommended):
Management Options (commonly referenced in clinical practice):
1. Basic Clinical Test
Pinch Test (Skin Turgor Test)
Method: Use your thumb and forefinger to lightly pinch the skin (commonly on the back of the hand or under the eye) for 5 seconds.
Interpretation:
2. Factors Affecting Elasticity
3. Professional Measurement Tools
4. Clinical Recommendations
Preventive Care:
Therapeutic Options:
Topical agents: vitamin C, peptides, antioxidants
1. Basic Clinical Observation
Visual Inspection: Skin texture refers to the smoothness and uniformity of the skin surface.
Common Characteristics:
2. Contributing Factors
3. Commonly Referenced Tools
4. Clinical & Preventive Considerations
Prevention (general measures):
Management (commonly referenced in dermatology):
Supportive care: Thermal-based devices (e.g., VASO Mask) may be incorporated to support circulation and overall skin health.
1. Basic Clinical Observation
2. Factors Affecting Wrinkle Formation
3. Professional Measurement Tools
4. Clinical Recommendations
• Age – Wrinkling, lentigines, and telangiectasia increase with age.
• Gender – Males show more wrinkling/telangiectasia; females influenced by
menopause and hormones.
• Ethnicity – Asians show more dyspigmentation; Europeans show earlier wrinkling.
• Hormonal – Menopause affects skin aging, though findings remain mixed.
• Nutrition – Higher vegetable and fatty acid intake reduces wrinkles/dryness.
• Sleep – Good sleep quality linked to reduced skin aging.
• Sunscreen – Use reduces wrinkling and photoaging.
• Smoking – Strongly accelerates wrinkling (“smoker’s face”).
• Air Pollution – Linked to lentigines, wrinkles, sagging.
• Lifestyle – Stress and sleep deprivation cause wrinkles, droopy eyelids.
• Alcohol – High intake (>40 g/day) strongly linked to wrinkles.
Discuss extrinsic and intrinsic aging factors
• Moisturizer / Hydration → e.g., hyaluronic acid, aloe vera, ceramides
• Sunscreen (SPF 30+) → broad-spectrum, daily use
All of Stage 1 Plus (+ –)
• Antioxidants Vitamin C, Vitamin E, Niacinamide (B3)
• Aesthetic non-invasive procedures → e.g., chemical peels and Hydrafacial for gentle skin renewal
All of Stage 1,2 treatment,plus
• Injectables and Dermal fillers
• Thermal energy that heats the dermis Intense pulsed light (IPL), Radiofrequency (RF) and Laser
All of Stage 1,2,3 treatment,plus
• Plastic surgery→ (e.g., facelifts or eyelid surgery)
• Hormone replacement therapy (HRT)